Gastroenterology Fellowship

Gastroenterology Fellowship Program
Application Opens | July 2, 2025
Next Start Date | July 1, 2026
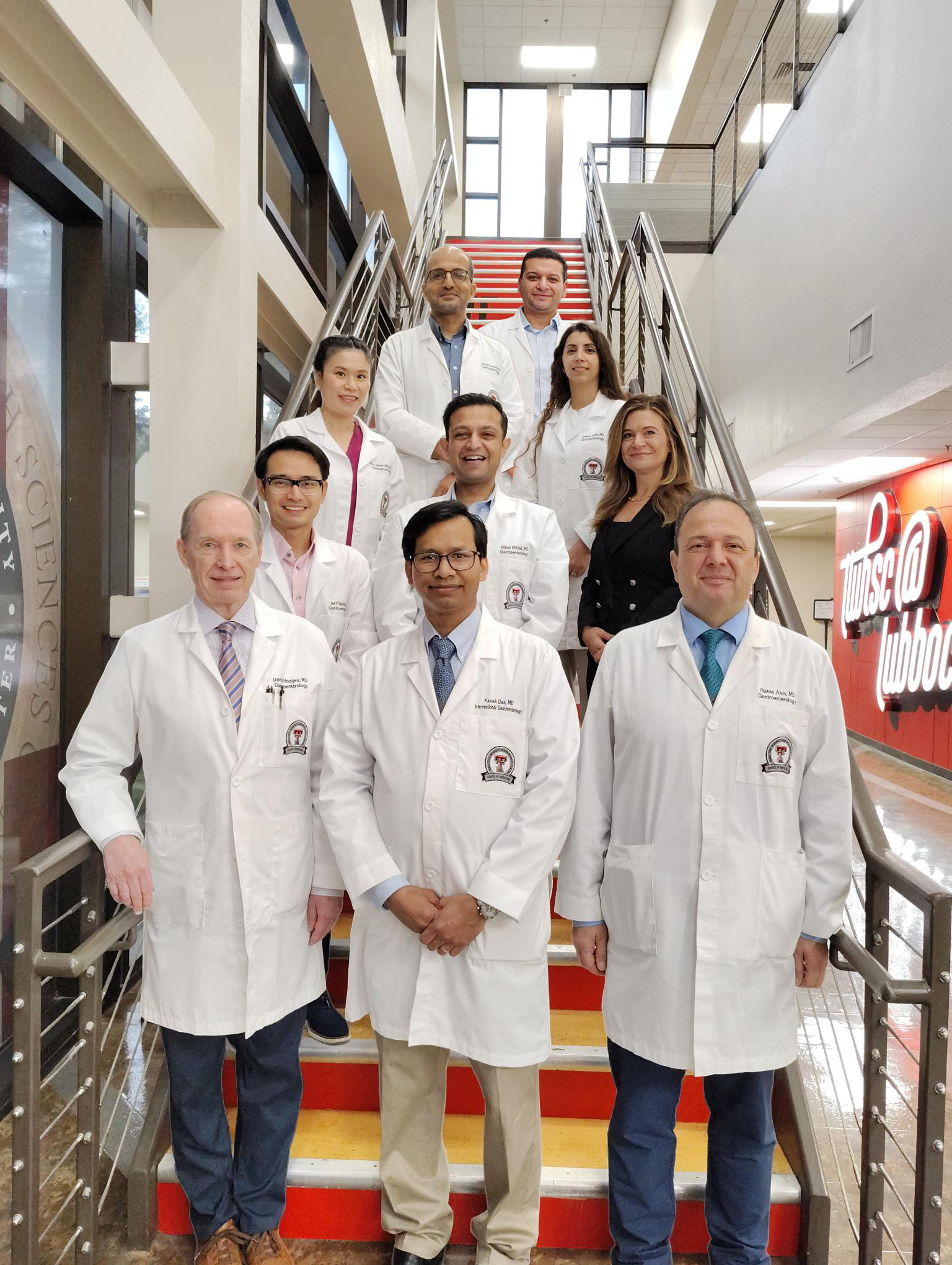
The Gastroenterology Fellowship program at Texas Tech University Health Sciences Center Lubbock was accredited in 2021, and the inaugural class of two fellows began training July 1, 2022. The goal is to train and retain physicians to practice in the surrounding West Texas communities.
The primary training site for endoscopy and inpatient consultation services is University Medical Center, a Level I Trauma Center, nonprofit county-owned hospital. At the end of training, the fellow will have met the requirements of the American Board of Internal Medicine (ABIM) for eligibility for the admission to the gastroenterology examination. Our program graduates possess the knowledge, skills, clinical judgment, attitudes and values of professionalism essential to the practice of gastroenterology.
Mission
The goal and the mission of our GI fellowship program is to provide a sound knowledge of broad spectrum of gastrointestinal, pancreaticobiliary and liver disorders, train the fellows with excellent clinical skills to prepare them for independent practice either in an academic setting or a private practice setting, to nurture the intellectual and innovative abilities of our fellows through the scholarly activities and to prepare them for future leadership roles in GI societies. The program expects that at the end of the three-year fellowship our fellows will achieve a high degree of professionalism and competency in clinical skills and clinical reasoning of general and complex GI and pancreaticobiliary and hepatic disorders and be successful in ABIM GI board certification examination.
Information for Applicants
Application Process and Eligibility Criteria
Applications are accepted through ERAS (Electronic Residency Application Service) only. We participate in the NRMP Match and will accept applications for the fellowship through August 15. Applications will be reviewed and then selected applicants will be contacted to schedule interviews. Inquiries concerning the Gastroenterology Fellowship can be directed to Tracy Treviño.
Application Check List:
- ERAS Application
- ERAS Addendum Form (only needed upon invitation for an interview)
- Curriculum Vitae (in chronological order with no gaps)
- MSPE
- Medical School Transcript
- USMLE/Complex Scores
- A minimum of (3) Letters of Recommendation
- Personal Statement
- Notarized copy of Diploma (only needed upon invitation for an interview)
- Copy of State License (only needed upon invitation for an interview)
Attention: At present, this program is not accepting away rotator applications. Kindly revisit this page periodically for any updates.
Salaries
*These amounts are for the Lubbock Campus only. Please contact TTUHSC Amarillo and TTUHSC Permian Basin for their salary information.
| Year | PGY1 | PGY2 | PGY3 | PGY4 | PGY5 | PGY6 | PGY7 |
|---|---|---|---|---|---|---|---|
| 2025-2026 | $65,764.23 | $67,250.96 | $69,374.62 | $72,532.94 | $74,685.79 | $76,841.81 | $78,997.84 |
| 2024-2025 | $63,725.03 | $65,165.66 | $67,223.47 | $70,283.84 | $72,369.95 | $74,459.12 | $76,548.30 |
| 2023-2024 | $61,570.07 | $61,570.07 | $64,950.21 | $66,936.99 | $68,923.76 | $70,913.45 | $72,903.14 |
| 2022-2023 | $58,918.73 | $60,250.71 | $62,153.31 | $64,054.53 | $65,955.76 | $67,859.76 | $69,763.77 |
| 2021-2022 | $57,202.65 | $58,495.83 | $60,343.02 | $62,188.87 | $64,034.71 | $65,883.26 | $67,731.82 |
| 2020-2021 | $55,536.56 | $56,792.07 | $58,585.46 | $60,377.54 | $62,169.63 | $63,964.33 | $65,759.05 |
Additional Benefits Include:
- Malpractice Insurance
- Aggregates are $100,000 per incident and $300,000 annual aggregate. Professional Liability Division website or call 806.743.9921
- Health Insurance
- Group Health/Dental/Vision insurance for residents and eligible dependents.
- Workers' Compensation
- Vacation
- Vacation is approved for not more than 15 working days for PGY 1 and 2 and not more than 20 working days for PGY-3 and above.
- Leave
- Sick leave for up to 12 working days per year
- Family and parental leaves of absence (see also US Department of Labor Employment Standards Administrative - FMLA)
- Educational leave
- Military leave not to exceed 15 work days per year.
- Retirement & Savings
- Residents and fellows are not eligible for TTU System's 401K plan but can participate in the Optional Retirement Program (ORP) the Tax-Deferred Account Program (TDA). More information will be provided upon starting your program.
Specific information pertaining to benefits is found in the House Staff Policies and Procedures.
Clinical Rotation & Block Scheduling
First Year: PGY4
- Inpatient rotation/consult: 7 months
- Outpatient: 2 months
- Research: 1 month
- Hepatology: 1 months
- Elective: 1 month
Second Year: PGY5
- Inpatient rotation/consult: 5 months
- Outpatient: 2 months
- Research: 1 month
- Hepatology: 1 month
- Elective: 3 months
Third Year: PGY6
- Inpatient rotation/consult: 3 months
- Outpatient: 4 months
- Research: 1 months
- Elective: 4 months
Inpatient/Consult:
This is a collaborative consultation service between Texas Tech Physicians and UMC
Physicians. We cover the hospital consults year-round. Our program does not have a
primary admitting service. Thus, GI is always a consultative service. Our goal is
to provide prompt consultation to expedite patient care. Our inpatient team consists
of fellows, residents, medical students, advanced practice providers (APP) and the
supervising physician. We strive to provide adequate autonomy and supervision to our
fellows and residents. It is expected that a fellow will also provide adequate supervision
and teaching to our residents and medical students. Currently, there are two fellows
in the rotation taking general and advanced GI consults. A third fellow may be added
in the future and would be dedicated to advanced GI consults. We are promised to provide
our fellows with diverse experiences with endoscopy and a wide range of general and
advanced GI disorders.
Our inpatient call schedule is friendly to a fellow’s well-being and learning. We comply with the ACGME work hour requirements. During the week one fellow takes after-hour consultations and this alternates between the two inpatient fellows for the entire month. Our weekend call begins on Saturday and ends on Monday morning. Weekend call is one every 6 weeks. Our hospital provides anesthesia support for almost all cases we perform. In addition, we are fortunate to have anesthesia availability on Sunday which allows us to take care of acute/emergent GI cases to expedite patient care and support our hospital system. Our main OR is also available 24/7 for any case that needs to be added on afterhours or if could not be accommodated in endoscopy suite. We are proud of our teaching friendly team all around.
Outpatient rotation:
During this rotation, fellows are assigned with six half day endoscopy blocks and
four half day ambulatory clinic (faculty clinic) blocks with a supervising physician
in each work week. The faculty clinics include both general GI clinics with exposure
to bread-and-butter GI disorders, inflammatory bowel disease, GI dysmotility etc.
and advanced GI clinics with exposures to various advanced endoscopy related cases
such as achalasia, gastroparesis, evaluation for resection of large colon polyps by
EMR or ESD, endoluminal stenting, various biliary and pancreatic disorders, and evaluation
for EUS, ERCP and other EUS guided therapies. This rotation provides a fellow with
ample exposure to a wide range of GI disorders and endoscopy experiences. Fellows
will also learn how to interpret high resolution esophageal manometry, pH monitoring/
Bravo study, and Video capsule endoscopies.
Elective rotation:
This rotation is an open-ended rotation and created keeping fellows future practice
interests in mind. This rotation can be customized based on a fellow’s future training
preferences such as advanced endoscopy (AE), motility disorders, IBD and transplant
hepatology. If a fellow wants to pursue an advanced endoscopy fellowship, this block
assures at least six months of advanced endoscopy rotation to prepare the fellow for
the AE fellowship. Fellows can also just choose to do all outpatient rotation if his/her
desire is to be a general gastroenterologist. The program is very flexible in this
regard. Our collaboration with regional liver transplant centers will provide a fellow
with a good exposure to transplant hepatology and may facilitate a future fellowship
if so desired. If a fellow elects to undergo dedicated IBD training or motility training,
the program/GME will facilitate at least one month of away rotation. If a fellow chooses
any of these tracks, the program leadership must be informed in advance to facilitate
the process. The program leadership understands the intricate relationship between
GI and other supportive services such as IR/body radiology, Pathology, bariatric surgery,
colorectal surgery and hepatopancreatic biliary surgery; and thus, one month (½ day
block, each day excluding weekends) each year is dedicated towards this ambulatory
rotation to enhance fellow’s understanding on GI radiology, pathology, bariatric,
colorectal, and hepatic pancreatic and biliary surgeries.
Hepatology/Transplant Hepatology Rotation:
The program understands that a strong knowledge in core hepatology is indispensable
in GI fellowship training. Our practice provides good experience in general hepatology.
However, to provide fellows with a dedicated hepatology and transplant hepatology
experience, the program is actively working on establishing an away rotation with
regional liver transplant centers where the program expects that a fellow will rotate
at least for three months during the fellowship training.
Continuity Care Clinic:
Each fellow will have one half day of continuity care clinic per week. The program’s
goal is to allow the fellows sufficient autonomy to boost their confidence in evaluating
and managing their patients longitudinally with minimum faculty supervision necessary.
A fellow typically evaluates seven to eight patients per clinic. When on inpatient
rotation, one fellow (7 am to 4 pm) gets clinic cancelled for the week, and the other
inpatient fellow (4 pm to 7 am) ends the clinic by 4 to ensure work life balance of
our fellows.
Research:
Ours is a newly accredited program. We aim to provide our fellows with the best scholarly
opportunities possible. The program fosters clinical and or basic research and any
scholarly activities a fellow can come up with. Fellows are required to produce at
least one, preferably three, scholarly activities during their fellowship training
in the form of either a case report, or case series or abstract at a national or international
conference or prospective or retrospective research study or meta-analysis and systemic
reviews. A fellow is assigned a total of four months of dedicated research time during
the fellowship training. The school of medicine established clinical research institute
(CRI) to foster research with full support needed. Fellows are encouraged to utilize
this support early in their research planning. It is also possible to assign a fellow
during this research rotation with an outpatient endoscopy block whenever available
and possible to keep the fellows’ endoscopy skills sharp.
Duration and Experience
Our fellowship program is a three-year program. We offer two fellowship positions per year. The fellows will rotate through the inpatient and outpatient settings. To enhance the core hepatology knowledge, in addition to the knowledge at our University Medical Center (UMC) hospital, fellows will rotate through regional renowned transplant hepatology programs, and this will provide an excellent experience in terms of management of various acute and chronic general liver disorders as well as liver transplant recipients. We have enough case volumes to competently train our fellows. We anticipate that at the end of fellowship each fellow will graduate with four to five times of the case volumes required per ACGME.
Procedural Experiences
The faculty at our program are trained to perform the following procedures which will expose the fellows to a wide range of GI endoscopy procedures to excel in their future independent practice.
- Esophagogastroduodenoscopy
- Total colonoscopy
- Flexible sigmoidoscopy
- Video capsule enteroscopy
- Push enteroscopy
- Single balloon enteroscopy
- High resolution esophageal manometry
- Wireless esophageal pH test (Bravo study)
- Fecal microbiota transplantation (FMT)
- Endoscopic mucosal resection (EMR)
- Endoscopic submucosal dissection (ESD)
- Endoscopic ultrasonography (EUS)
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Choledochoscopy (Spy glass examination of the bile duct), Electrohydraulic Lithotripsy (EHL)
- Pancreatoscopy
- Endoluminal stenting (esophageal, duodenal, and colonic)
- EUS guided celiac plexus block and neurolysis
- Other EUS guided interventions such as EUS guided bile duct access/drainage, EUS guided Gall bladder drainage, EUS guided cyst gastrostomy, and pancreatic necrosectomy etc.
- Per oral endoscopic myotomy (POEM)
- Third space endoscopy
Thank you for your interest in the Gastroenterology fellowship at the Texas Tech University Health Science Center in Lubbock, Texas. We welcome you to explore the details of our program within this webpage.
The Gastroenterology Fellowship program at Texas Tech University Health Sciences Center in Lubbock was accredited in 2021, and the inaugural class of two fellows began training July 1, 2022. Our fellowship program is a three-year program. We offer two fellowship positions per year and participate in the ACGME GI fellowship match.
The goal of our GI fellowship program is to provide a sound knowledge of broad spectrum of gastrointestinal, pancreaticobiliary and liver disorders; and train the fellows with excellent clinical skills to prepare them for independent practice either in an academic setting or a private practice setting. We strive to nurture the intellectual and innovative abilities of our fellows and prepare them for future leadership roles in GI societies. At the end of the three-year fellowship our fellows are expected to have achieved a high degree of professionalism and competency in clinical skills and clinical reasoning of general and complex GI and pancreaticobiliary and hepatic disorders.
Our fellowship program primarily operates at the University Medical Center, a Level 1 Trauma Center, nonprofit county owned hospital. The 510-bed hospital draws many acute cases from the surrounding communities. We have the diversity of GI pathologies and case volumes that will undoubtedly equip a fellow for future independent practice. Our practice serves a friendly community, and we hope that fellows will choose to serve our community at the end of the training.
The Texas Tech GI fellowship program participates in a unique yet strong collaboration with a group of academic gastroenterologists and private practice-oriented gastroenterologist which would allow the fellows to observe and be trained in both aspects of gastroenterology practice- academic and private.
Our curriculum is thoughtfully prepared to ensure required training for the fellows according to ACGME recommendations. Our didactic sessions are well planned and geared towards enhancement of fellows’ knowledge base and the ABIM- Gastroenterology board certification examination. Fellows and residents in our program enjoy autonomy in clinical decision making and play a remarkable role in clinical learning of the entire team including medical students.
We hope to work with you passionately to deliver the education and training you strive for.
If you are interested in receiving more information, please email your request to Tracy Treviño.
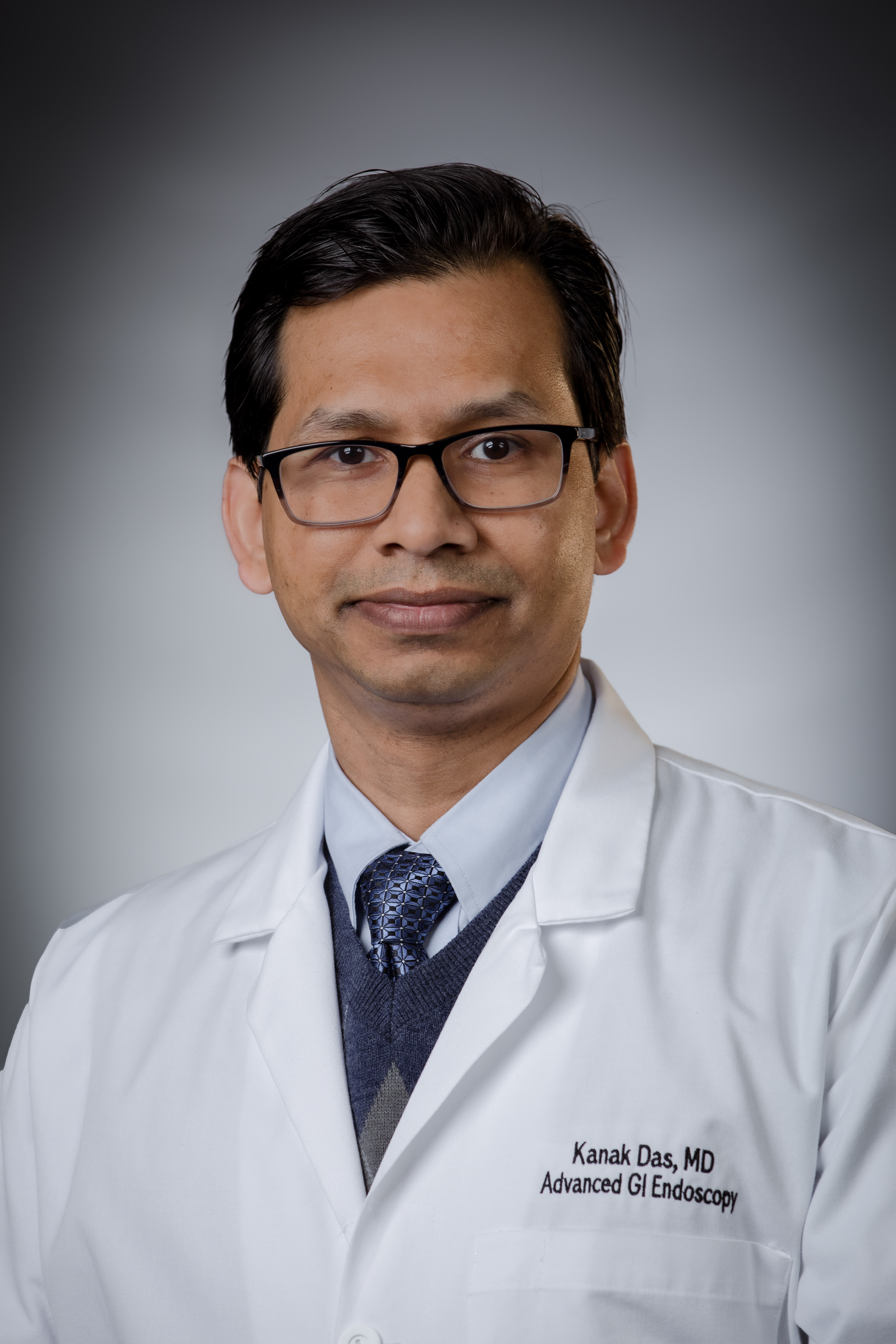
Kanak Das, MD
Professor; Dept. of Medicine
Program Director, Gastroenterology Fellowship
Interventional Gastroenterologist, Div. of Gastroenterology
Clinical Training Sites
Currently, the primary site of training for our program is the University Medical Center, a 510+ bed hospital with an excellent Level 1 Trauma center. This is the hospital where fellows get their majority of the experiences especially all acute care experiences. At this hospital, we have all the support needed to train our fellows with a sound knowledge in gastroenterology. We have excellent services from interventional radiology (IR), hepatobiliary and pancreas surgery (HPB), colorectal surgery (CRS), acute care surgery (ACS), medical and surgical oncology, nutrition, and intensive care units (ICUs). Our approach is multidisciplinary as we strive to provide comprehensive care for our patients.
Fellows get their outpatient experiences including outpatient endoscopy, ambulatory clinics, and fellows’ continuity care clinic at various locations. Outpatient endoscopy takes place at the UMC endoscopy suite as well as at the UMC’s GI and Outpatient services location which is a state-of-the-art endoscopy facility.
Fellows on outpatient rotation attend ambulatory clinics. These are private clinics of the attending physicians in the fellowship. These clinics provide excellent experience early in their career of various simple and complex GI and hepatobiliary and pancreatic disorders. Fellows’ continuity care clinic (half day clinic) is located at the Texas Tech Physicians Medical Pavilion and is held once a week. Fellows also get outpatient transplant hepatology experience once a month by rotating with esteemed hepatologist from UT Southwestern Medical Center, Dallas, TX.
To ensure a solid knowledge base on management of liver disorders, the program is actively working on establishing an away hepatology rotation at regional liver transplant centers and more updates to follow soon.
Teaching Sites
Texas Tech University Health Sciences Center
TTUHSC educates students, provides patient care and conducts biomedical and clinical research. We graduate the most health care professionals in the state of Texas. Nationally recognized for innovative programs, academic achievement, and our cutting-edge research, we are training the next generation of highly qualified health professionals. To date we have trained more than 42,000 health care professionals who are serving patients and driving medical discovery in tangible, life-changing ways – both for the 10 million people in our immediate service area and around the world.
University Medical Center (UMC) is a 500-bed hospital. It is a public, non- profit
facility that serves as the primary teaching hospital for the Texas Tech University
Health Sciences Center. UMC also includes a children's hospital
with Level IV NICU, a family-centered birth center, a regional burn center, and the
region's only Level 1 Trauma Center. Wile at UMC, TTUHSC Family Medicine residents
take care of hospitalized adults & children, work in the
critical care units, and provide family-centered maternity care in labor & delivery.
UMC Gastroenterology clinic at 4309 102nd Street in Lubbock, Texas, opened as part of the initiative to expand healthcare services in Southwest Lubbock. This clinic, along with UMC's Endoscopy Center, provides advanced gastrointestinal care to the region, offering both adult and pediatric gastroenterology services.
Vanessa Costilla, MD
Site Director, GI Fellowship
Dr. Vanessa Costilla is a gastroenterologist in Lubbock, TX and has over 13 years of experience in the medical field. Dr. Costilla is eager to fill the gaps of diversity in healthcare by being a female provider, and being bilingual, speaking both English and Spanish. She is passionate about partnering with her patients through their healthcare journey.
Education:
- Fellowship: Gastroenterology, University of Texas Health Science Center
- Residency: Internal Medicine, Mayo Clinic Hospital
- Medical School: Texas Tech University Health Science Center

Nebiyou Wondimagegnehu, MD
Participating Faculty
Dr. Nebiyou Wondimagegnehu is a gastroenterologist in Lubbock, Texas and is affiliated with multiple hospitals in the area. He has been in practice for more than 20 years. Dr. Nebiyou Wondimagegnehu has expertise in treating stroke, upper gi endoscopy, among many other conditions.
Education:
- Fellowship: Gastroenterology, Howard University Hospital Internal Medicine GME
- Residency: Internal Medicine, Texas Tech Health Sciences Center
- Medical School: Addis Ababa University
UMC’s Cancer Center is a nationally recognized leader in the fight against cancer. Our multi-disciplinary approach combines the expertise of Texas Tech physicians with UMC's compassionate care and technological advancements. Comprehensive cancer treatment and care is available in one facility, close to home.
The CC provides patients with a wide-range of treatment options, including chemotherapy, radiation therapy, surgical oncology and bone marrow transplant. Our team of physicians includes experts in medical, surgical and pediatric oncology, as well as hematological diseases. The first Bone Marrow Transplant Unit in the region was started right here at UMC, and the first clinical trials offered in the West Texas region began here, too.
Covenant Health Facilities
Throughout our region, wherever there’s a need, Covenant Health is there to help.
At our flagship facilities in Lubbock — Covenant Medical Center and Covenant Children’s
— we house a number of specialty treatment centers, including:
Lubbock Digestive Disease Associates (LDDA)
Since 1986, LDDA's mission has been to provide quality, cost-effective care to our
patients in an atmosphere of professional dedication and compassion. With physicians
at LDDA who are trained in internal medicine and gastroenterology, you can expect
the high-quality treatment you depend on when you need it.

Ariwan Rakvit, MD
Site Director, GI Fellowship
Dr. Ariwan Rakvit is a board-certified gastroenterologist with Lubbock Digestive Disease Associates. She performs routine GI procedures such as upper endoscopy, colonoscopy and capsule endoscopy in the diagnosis, screening and surveillance of gastrointestinal diseases and cancers. She is particularly interested in colon cancer screening and gastroesophageal reflux disease. In addition, she also specializes in liver disease, including hepatitis and cirrhosis. She is fluent in English, Thai and Mandarin. She is a member of the American College of Gastroenterology, American College of Physician and American Gastroenterological Association.
Education:
-
Graduate School: Chulalongkorn University, Bangkok, Thailand
-
Medical School: Chulalongkorn University, Bangkok, Thailand
-
Residency: Texas Tech University Health Science Center
-
Fellowship: SUNY Upstate Medical University
University of Texas Health Science Center at San Antonio
Fellows participate in a one month away rotation during their first year of training through the inpatient and outpatient hepatology and transplant hepatology services with direct involvement in patient care and calls. This site provides high quality education, experience, and research in a wide spectrum of general hepatology disorders and liver transplantation.
Fred Poordad, MD
Site Director
Dr. Poordad is Clinical Professor of medicine at the University of Texas Health Science Center, San Antonio, and Vice President of Academic and Clinical Affairs at The Texas Liver Institute in San Antonio. Dr. Poordad received his bachelor and medical doctorate at the University of Alberta in Edmonton and completed a residency in internal medicine at St. Thomas Medical Center and Northeastern Ohio Universities College of Medicine. Dr. Poordad also completed fellowships in gastroenterology at the University of South Carolina and in hepatology/liver transplantation at the Johns Hopkins University School of Medicine. Dr. Poordad served as the co-director of liver transplantation at Johns Hopkins prior to becoming chief of hepatology and liver transplantation at Cedars-Sinai Medical Center in Los Angeles for 10 years. In 2012, he joined The Texas Liver Institute and the faculty at the University of Texas Health Science Center in San Antonio. He teaches medical students, resident and fellows and rotates on the liver transplant services at University Hospital System. Dr. Poordad also conducts a multitude of clinical research across all facets of liver disease, including viral hepatitis, fatty liver and cirrhosis.
University of Texas Southwestern Medical Center
Fellows participate in a one month away rotation during their second year of training through the inpatient and outpatient hepatology and transplant hepatology services with direct involvement in patient care and calls. This site provides high quality education, experience, and research in a wide spectrum of general hepatology disorders and liver transplantation.

Ariel Aday, MD
Site Director
Ariel Aday, M.D., is an Assistant Professor in the Department of Internal Medicine at UT Southwestern Medical Center, and a member of the Division of Digestive and Liver Diseases. She serves as the Program Director of the Gastroenterology Fellowship Program. Her research interest is medical education.
Originally from Bristol, Virginia, Dr. Aday holds a bachelor’s degree in biology from the University of North Carolina and earned her medical degree at Wake Forest University School of Medicine in Winston-Salem. She completed internal medicine residency training at UT Southwestern, where she also served as Chief Medical Resident. She remained at UT Southwestern to complete her gastroenterology fellowship.
Board certified in internal medicine and gastroenterology, Dr. Aday initially joined the UT Southwestern faculty in 2015 as an Assistant Instructor during her tenure as Chief Medicine Resident. She rejoined the faculty in 2019 and quickly resumed her involvement as a GME leader.
Board Review - Emphasis is on board testing techniques and review of multiple-choice questions.
House Staff Meeting - is a monthly meeting of all TTUHSC residents sponsored by the office of GME. This meeting serves to update house staff on important institutional issues. Elected officers of the house staff serve as liaisons on many institutional committees.
Case Conference - A case is prepared by a fellow in advance of the conference. The fellow delivers a brief, updated aspect of the presentation topic.
Pathology and Radiology Conference - These cases based didactic sessions cover core topics in gastrointestinal pathology and core principles of interpretation of gastrointestinal imaging students. Sessions are co-led by a gastroenterology fellow and a pathologies/radiologist.
Patient Safety - Cased-based medical conference that emphasizes challenges or adverse outcomes associated with system interactions in medical care.
Journal Club - These sessions review seminal new research articles in gastroenterology and hepatology. Fellows will present articles along with a faculty member to help guide discussion on how the findings from these articles may influence practice. Each session had a dedicated topic throughout the academic year (i.e. hepatology, motility, luminal gastroenterology, inflammatory bowel disease, small bowl, or pancreaticobiliary diseases.
Grand Rounds - These are conducted by the Department of Medicine and other institutional faculty as well as visiting professors. Topics include advances in basic and clinical knowledge in many fields in Internal Medicine and its subspecialties.
Morbidity and Mortality - is conducted by the Department of Medicine faculty as well as visiting professors and is a noon conference series where residents/fellows present specific cases for presentation under the supervision of a faculty member.
Core Conference - These didactic sessions cover core topics in gastroenterology and hepatology. Sessions are led by faculty from TTUHSC, UMC, and private community physicians in their areas of clinical or research expertise.
See what Lubbock has to offer!
Lubbock, home to over 252,500 residents and Texas Tech University’s 36,550 students, blends the energy of a thriving city with the charm of a cozy college town. Known worldwide as the birthplace of rock pioneer Buddy Holly, the city offers world-class arts, museums, entertainment, and a vibrant cultural scene. Outdoor enthusiasts enjoy abundant sunshine, recreational lakes, top-ranked golf courses, and easy access to hiking, fishing, and camping in nearby New Mexico. With a strong economy, low housing costs, excellent schools, and the High Plains wine region nearby, Lubbock is a dynamic hub for culture, education, and adventure.
Explore life in Lubbock and see why it’s a great place to live, work, and play here.
Got Questions?
We're here to help. Contact us if you have questions.
Kanak Das, MD
Program Director, Gastroenterology Fellowship
Professor, Department of Medicine
Interim Chief, Division of Gastroenterology
Interventional Gastroenterologist, Division of Gastroenterology
Education
- Medical School: Chittagong Medical College, Bangladesh
- Residency: Internal Medicine, University of Tennessee Health Science Center
- Fellowship: Gastroenterology, University of Tennessee Health Science Center
Hakan Akin, MD
Professor, Department of Medicine
Gastroenterologist, Division of Gastroenterology
Education
- Medical School: School of Medicine, Hacettepe University, Ankara, Turkey
- Residency: Internal Medicine, Marmara University, Istanbul, Turkey
- Fellowship: Gastroenterology, Marmara University, Istanbul, Turkey
- Fellowship: Transplant Hepatology, University of Texas Health Science Center at San Antonio
David Hodges, MD
Clinical Professor, Department of Medicine
Division of Gastroenterology
Education
- Medical School: Texas Tech University
- Residency: Internal Medicine, Texas Tech University Health Sciences Center
- Fellowship: Gastroenterology, Texas Tech University Health Sciences Center

Tracy Treviño
Program Coordinator, Gastroenterology & Nephrology Fellowships
Phone: 806.743.9886
Fax: 806.743.3143
3601 4th St. MS 9410
Lubbock, TX 79430
